What are the Symptoms and Causes of IBS?
- Treatments, Testing and Diagnosis
Maybe you’ve noticed a new symptom that comes with your IBS – back pain. As if there weren’t enough already!
In this article I will explain what the symptoms of IBS are and also what the causes of IBS can be. These are two confusing topics which you will need to understand in order to control your condition.
If you have IBS, you may already experience a range of symptoms. These can be very different to someone else you know who has IBS too. So, it could be quite alarming if you have back pain and IBS when someone else does not.
Similarly, you may be looking for answers about why you have this problem in the first place.

How to get an IBS diagnosis
Please note that IBS symptoms are not enough to give an accurate diagnosis. Many IBS symptoms are similar to other digestive conditions such as coeliac disease, inflammatory bowel disease and even bowel cancer.
To ensure you have had the correct diagnosis, you need certain tests done. These tests will rule out other health conditions.
To get more information on the exact tests required for an IBS diagnosis please see our other blog post here.
IBS symptoms
You may be familiar with what symptoms you are experiencing and suspect they could be related to IBS. Let’s go over some of the most commonly reported symptoms with IBS.
1. Bloating
Bloating is a very common symptom of IBS. Bloating is caused by excess gas and wind that is trapped in the abdomen causing that swollen tummy that often coincides with pain and discomfort.
You can read more here about bloating, along with tips for instant relief.
3. Stomach cramps and abdominal pain
This is the key diagnostic symptom for IBS, if you experience abdominal pain for at least one day of the week (1).
A gut that has IBS is hypersensitive. What this means is that, in response to normal digestion, the gut is signalling to the brain to feel pain.
3. Excess Gas
Gas production is a normal product of digestion. However as a result of having IBS, excess gas may be produced. This is due to change in bacteria in the gut and possible food intolerances.
4. Diarrhoea
Diarrhoea is defined as the passage of three or more loose or liquid stools per day (or more frequent passage than is normal for the individual) (2).
Diarrhoea can be caused by food intolerances and hypersensitivity. Dietary triggers such as FODMAPs, caffeine, nicotine, alcohol intake and spicy food can also cause diarrhoea (3).
5. Loose stools
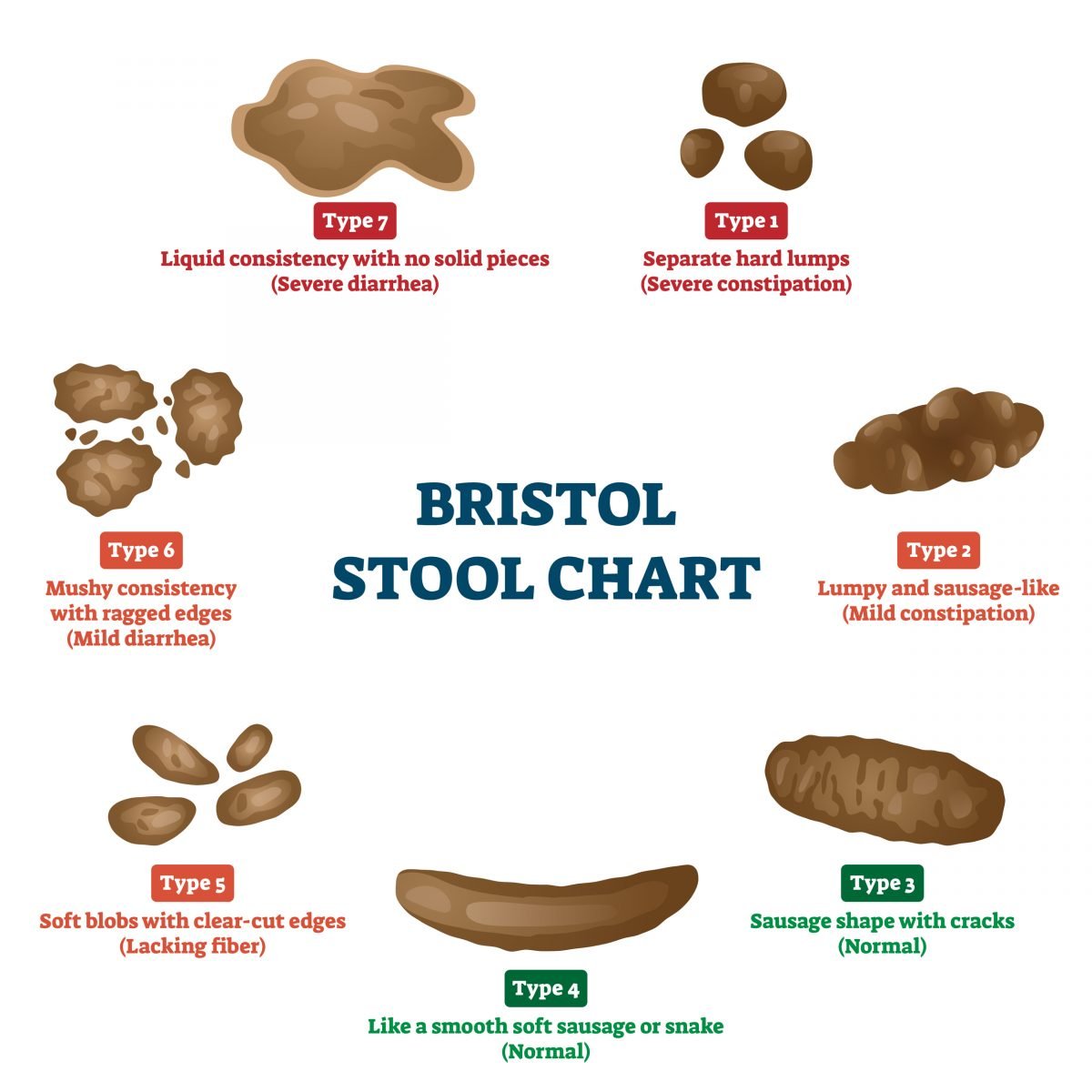
Have you noticed that your bowels are in between diarrhoea and being normal? This would still be classified as diarrhoea predominant IBS (IBS-D). Take a look at the stool chart below – if stools are types 5 or 6, then you would still be classed as this type.
6. Constipation
Constipation can look different for everyone, but generally can be identified as hard lumpy stools and require severe straining. Bowels will not open as easily as they should and open less than three times a week (4).
7. Fatigue
If you feel exhausted then this may be a symptom of your IBS (5).
When you feel tired with IBS, the causes are likely due to a combination of factors. Regular pain, bloating, constipation and diarrhoea will all make you feel fatigued. Understandably!
You may also feel quite stressed and low in mood about your symptoms. Stress and a low mood have also been linked to fatigue.
You can read more here about “Does IBS cause fatigue?”.
8. Low mood and anxiety
Mental health is connected to IBS through something known as the gut-brain axis (6).
So, it is not surprising that you may feel lower in mood or suffer from anxiety.
In one paper, it was even suggested that people with anxiety and depression are twice as likely to suffer with IBS. Prevalence of anxiety and depression in clinical samples with gastrointestinal disorders is 60-85% (7).
Is back pain a symptom of IBS?
We added this section as the term ‘back pain and IBS’ is commonly searched for in google. This is a clear sign that many people are wondering if the two are linked.
Back pain is not considered a symptom of IBS and has not been linked in research. So if you are experiencing IBS then you must speak to your doctor rather than assuming it is related to your IBS.
Back is a common complaint. So the chances of you having both IBS and back pain are high. But there is no research showing that IBS causes back pain and so you should not presume that your back pain is linked to your IBS.
What causes IBS?
You will be frustrated to find that the exact cause of IBS is currently unknown. Research does show that IBS causes could be multifactorial.
Have you ever been told ‘it is all in your head’? As nasty as this comment is, there may actually be some truth to it. When we look at IBS pain symptoms, research suggests that it could be due to a sensitive nervous system.
If we have a hypersensitive gut, this signals pain to our brain when nothing out of the ordinary is going on with your gut (8).
The following issues are said to be related to causes of IBS (9):
- Stress
- Infection
- Being female
- Food intolerances
Psychological factors
When our body is under stress, it releases a hormone called cortisol. Cortisol is known to play havoc with our digestive system and is often coined the “stress hormone”.
When released, cortisol acts to direct blood to the brain, other organs and larger limbs, away from the digestive system. Stress also disrupts the gut permeability and function, changing how pain is signalled to the brain (10).
It may be a good time to check in with your stress levels, simple changes to managing stress could go a long way in managing your IBS.
Can IBS be cured?
While you can manage your IBS symptoms, there is currently no proven cure. This means that IBS is a ‘chronic’ condition.
How can I manage my IBS?
Below I have listed out different, scientifically proven ways to manage IBS. Even though each method is proven to aid manage IBS symptoms, it is recommended to try them all. IBS is a multifaceted condition and needs a full 360 degree approach.
The Low FODMAP diet
‘FODMAPs’ stands for fermentable oligosaccharides, disaccharides , monosaccharides and polyols. The low FODMAP diet has been shown to have up to a 70% effective rate at managing IBS symptoms (11).
FODMAPs are different types of carbohydrates and therefore found in different types of foods. Don’t panic! This does not mean you need to cut out all carbohydrates from your diet to manage your IBS, this is never recommended by a health professional.
FODMAPs travel through your digestive system to the large intestine, where they are broken down by natural gut bacteria.
This process is called fermentation, producing gas that draws water into your large bowel. In those with IBS, this process of fermenting FODMAPs can cause the symptoms already mentioned previously (12).
To find out exactly what a Low FODMAP diet is, click here.
Probiotics
Have you ever been told, you need to take probiotics to help your gut? There is some truth behind this.
For more information on what probiotics are and which type of probiotic you can take for your IBS, read here.
Psychological
I’m sure by now it is no surprise that managing your IBS will come with a psychological element.
Cognitive behavioural therapy (CBT), hypnotherapy and mindfulness have all shown to have benefits when managing IBS symptoms (13). If you believe your IBS to be stress related, this will be particularly important for you. Although, general stress management is still very valuable.
Yoga
Research found that doing yoga twice a week saw reductions in their IBS symptoms just as much as being on a low FODMAP diet (14).
If you’re thinking about increasing your exercise or are already a gym bunny yourself, you may be interested in this blog post about how exercise effects gut health.
Fibre
If you have IBS-C then taking a fibre supplement can help to relieve symptoms.
But, be careful that you take the correct type of fibre supplement, only Psyllium, methylcellulose, calcium polycarbophil and wheat dextrin have been shown to reduce symptoms (15).
To find out more about fibre in the diet and IBS read more here.
Medication
Medications are usually not the first point of call for IBS symptom management. Usually taking a food first approach is the best way. In certain situations and after speaking to your doctor, medications are appropriate and there are some available.
To find out which medications are suitable for IBS management, read here.
Peppermint oil
You might like the taste of peppermint tea and hope that could be helping with your IBS symptoms. However, to get the full benefit of peppermint the best form is in oil and capsulated. This post provides recommendations for taking peppermint oil to manage your IBS symptoms.
Summary
The symptoms of IBS vary in type and intensity for different people. It is important to get an accurate diagnosis to ensure you get the appropriate help.
The causes of IBS are still very much unknown with no cure at present. The wide range of management strategies conveys how multifaceted the condition is and how a multifactorial approach is required,
However, by pinpointing triggers in the diet, targeting your gut microbiota and making some small lifestyle changes, your IBS can be manageable.
Article written by Camilla Donaldson BSc Hons Nutrition reviewed by Kirsten Jackson